
Just when you thought that hot flashes were enough to worry about during menopause another consideration is high cholesterol. High cholesterol is a risk factor for cardiovascular disease, the leading cause of death in women after menopause.
Our estrogen levels decline during menopause. Besides its heart-protective benefits, we need estrogen to help:
- Reduce inflammation in our blood vessels and help relax and widen them to improve blood flow.
- Reduce the buildup of fatty plaque in your arteries in order to maintain a healthy cholesterol profile.
- Neutralize harmful free radicals, which can damage cells and contribute to the development of heart disease.
Lower estrogen levels, along shifting hormones such as testosterone and progesterone during menopause, can impact your entire lipid profile, leading to high cholesterol and more.
It is recommended to get a lipid panel done at least once per year.. Lipids are fats stored in your body. Your lipid profile will typically include:
- High-density lipoprotein (HDL)
- Low-density lipoprotein (LDL)
- Total cholesterol
- Triglycerides
Cholesterol and Triglycerides need lipoproteins, (high-density lipoprotein (HDL) and low-density lipoprotein ( LDL) to transport them safely to cells and other areas where the body needs them.
HDL collects extra fats floating around in your blood vessels and takes them back to the liver, where they can be processed and eliminated. LDL, on the other hand, drops fat into your blood vessels. Too many deposits mean that those fats can build up and potentially form blockages, restricting blood flow to your heart.
Why Do Cholesterol Levels Increase Around Menopause?
When estrogen levels go down, other hormones quickly follow, and your entire lipid profile can shift. Your total cholesterol, LDL, and triglycerides may increase, while HDL can decrease. To be fair, menopause does not cause high cholesterol, but it can increase your risk.
These other factors that occur during menopause contribute to fluctuating lipid levels.
1. Weight Gain
Lower estrogen levels mean that fat can more easily be stored in your abdominal area. This dangerous fat (called visceral fat), can increase cholesterol levels and create other metabolic issues.
2. Insulin Resistance
One of estrogen’s roles is to maintain healthy blood-sugar levels. Insulin resistance can come about when our estrogen levels decline during menopause. Insulin is a hormone that helps regulate blood-sugar levels. When the body becomes resistant to insulin, it can lead to higher blood sugar, increasing LDL and triglycerides.
Research shows that insulin resistance can also contribute to menopausal symptoms like hot flashes.
3. Liver Health
Your liver metabolizes cholesterol and other lipids, helping make and eliminate excess amounts. Estrogen protects your liver by promoting the breakdown and removal of LDL from the bloodstream.
Our estrogen levels decrease during menopause, and our liver works harder to remove excess LDL cholesterol, which can lead to an imbalance in cholesterol levels.
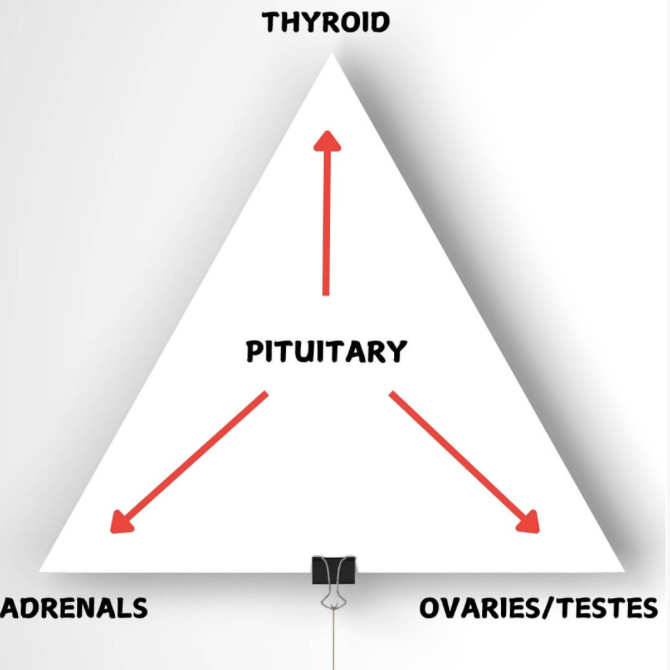
4. Thyroid Dysfunction
Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), help regulate your body's metabolism. Those hormones influence cholesterol-managing organs, such as your liver.
Menopause can trigger or exacerbate hypothyroidism, a condition where the thyroid gland doesn't produce enough thyroid hormones. When your body's metabolic rate slows down, things tend to get sluggish, and your body may not clear cholesterol from your bloodstream as easily and LDL levels increase.
Hypothyroidism can cause insulin resistance and weight gain.
5. Muscle Loss
Muscle plays a crucial role in regulating various metabolic processes, including how your body handles cholesterol. Muscle is a metabolically active organ, regulating lipid levels. It can utilize fatty acids for energy, for one, helping balance triglyceride levels.
These and other changes during menopause can impact your lipid profile, increasing LDL cholesterol and triglycerides while lowering HDL cholesterol.
1. Diet matters!
A high-sugar-impact diet with bad fats increases the small, dense, artery-damaging cholesterol particles and lowers the number of big fluffy harmless ones. A low-sugar-impact diet has the opposite effect, supporting healthy cholesterol levels.
Be sure to include protein and fiber in every meal. Optimal protein helps stabilize your lipid profile, balance blood sugar, support your metabolism, and help you stay at your goal weight.
2. Resistance Training
Resistance training can improve your overall lipid profile by lowering inflammation, decreasing total cholesterol, triglycerides and LDL, while improving HDL. Strength training can also improve hormones like adiponectin. This hormone’s anti-inflammatory and antioxidant benefits help regulate blood sugar levels and lipid metabolism.
3. Sleep matters!
Quality sleep helps manage inflammation, balance hormones, improve insulin sensitivity, and support the body’s stress-management abilities—all of which impact your lipid profile. Try to get at least seven to eight hours of quality, uninterrupted sleep every night.
4. Try and manage your stress.
Research shows that stress can be a risk factor for lipid disorders, such as high cholesterol and high triglycerides. Manage stress by practicing mindfulness, meditation and breathwork. Magnesium, Rhodiola, and Lemon Balm are supplements that may help.
A functional medicine health coach is invaluable during menopause because they provide personalized guidance, support, and holistic strategies to help women manage the complex array of physical and emotional changes that occur during this life transition.
If you have a particular issue you would like addressed through functional medicine and are interested in working together, or if simply wish to learn more, you can schedule a complementary discovery call with me!
1. Currie H, Williams C. Menopause, Cholesterol and Cardiovascular Disease, US Cardiology 2008;5(1):12–4.
2. Tuomikoski P, Ylikorkala O, Mikkola TS. Menopausal hot flashes and insulin resistance. Menopause. 2012 Oct;19(10):1116-20. doi: 10.1097/gme.0b013e3182503d5d. PMID: 22668816.
2. Tuomikoski P, Ylikorkala O, Mikkola TS. Menopausal hot flashes and insulin resistance. Menopause. 2012 Oct;19(10):1116-20. doi: 10.1097/gme.0b013e3182503d5d. PMID: 22668816.
3. Gierach M, Gierach J, Junik R. Insulin resistance and thyroid disorders. Endokrynol Pol. 2014;65(1):70-6. doi: 10.5603/EP.2014.0010. PMID: 24549605.
4. Lee JH, Lee HS, Cho AR, Lee YJ, Kwon YJ. Relationship between muscle mass index and LDL cholesterol target levels: Analysis of two studies of the Korean population. Atherosclerosis. 2021 May;325:1-7. doi: 10.1016/j.atherosclerosis.2021.01.016. Epub 2021 Jan 31. PMID: 33857762.
5. Prabakaran S, Schwartz A, Lundberg G. Cardiovascular risk in menopausal women and our evolving understanding of menopausal hormone therapy: risks, benefits, and current guidelines for use. Ther Adv Endocrinol Metab. 2021 Apr 30;12:20420188211013917. doi: 10.1177/20420188211013917. PMID: 34104397; PMCID: PMC8111523.
6. Surampudi P, Enkhmaa B, Anuurad E, Berglund L. Lipid Lowering with Soluble Dietary Fiber. Curr Atheroscler Rep. 2016 Dec;18(12):75. doi: 10.1007/s11883-016-0624-z. PMID: 27807734.
7. Costa RR, Buttelli ACK, Vieira AF, Coconcelli L, Magalhães RL, Delevatti RS, Kruel LFM. Effect of Strength Training on Lipid and Inflammatory Outcomes: Systematic Review With Meta-Analysis and Meta-Regression. J Phys Act Health. 2019 Jun 1;16(6):477-491. doi: 10.1123/jpah.2018-0317. Epub 2019 Apr 25. PMID: 31023184.
8. Xing C, Huang X, Zhang Y, Zhang C, Wang W, Wu L, Ding M, Zhang M, Song L. Sleep Disturbance Induces Increased Cholesterol Level by NR1D1 Mediated CYP7A1 Inhibition. Front Genet. 2020 Dec 23;11:610496. doi: 10.3389/fgene.2020.610496. PMID: 33424933; PMCID: PMC7793681.
9. Assadi SN. What are the effects of psychological stress and physical work on blood lipid profiles? Medicine (Baltimore). 2017 May;96(18):e6816. doi: 10.1097/MD.0000000000006816. PMID: 28471984; PMCID: PMC5419930.
10. Gisèle Pickering, André Mazur, Marion Trousselard, Przemyslaw Bienkowski,Natalia Yaltsewa, Mohamed Amessou, Lionel Noah, and Etienne Pouteau Magnesium Status and Stress: The Vicious Circle Concept Revisited.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7761127/
11.Andrew Scholey, Amy Gibbs, Chris Neale, Naomi Perry, Anastasia Ossoukhova, Vanessa Bilog, Marni Kras, Claudia Scholz, Mathias Sass, and Sybille Buchwald-Werner Anti-Stress Effects of Lemon Balm-Containing Foods https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4245564/









0 Comments